On Friday, 4th March, 2022; Men Of the Night Uganda launched a new program called the Anal pap smear for anyone that engages in anal sex regardless of their gender identity. An anal pap smear is a test that examines a small sample of cells for abnormal growth that could progress to cancer.
Women are advised to go for regular cervical cancer screening to the extent that this service has been made compulsory in schools for girls Primary 4 upwards but a man having a pap smear is almost unheard of or checking these same women being asked to scree for cervical cancer for anal cancer. Interestingly, the same virus human papilloma virus (HPV) that causes cervical cancer in women is responsible for causing anal cancer in men. The fact is that gay and bisexual men are at a much higher risk of anal HPV, which puts them at an increased risk for anal cancer. The risk is even higher in HIV positive gay and bisexual men. When compared to the general population, some studies have put the risk for anal cancer at 35 times greater for HIV negative MSM and 80 times greater for HIV positive MSM. The good news is anal cancer is both preventable and treatable if caught early. It is on this background of research and the prevalence of anal cancer in the MSM community that MONU has introduced the anal pap smear. This procedure is performed by taking a sample of cells from the anus that are then examined under a microscope in a lab. It is important to note that is not a diagnostic test but one that rather looks for precancerous or cancerous cells. If abnormal cells are found, further testing will be necessary. The anal Pap smear does not test for colon or rectal cancer and is he counterpart of the cervical Pap smear, which is named after George Papanicolaou, the Greek doctor who invented the test in the 1940s.
“Pap smears have been highly effective as a (cervical cancer) screening tool for women, so why not do the same thing for the anal canal?” Says Peter Leone, MD infectious Diseases expert at UNC medical center. Performing anal Pap smears is a valuable tool to detect cytologic changes associated with some strains of HPV infection. For persons participating in receptive anal intercourse, this diagnostic procedure provides the opportunity for early detection to guide appropriate follow-up and interventions. We want appropriate screening to be incorporated easily into a primary care practice especially among high-risk groups that would benefit from this screening which include men who have sex with men, HIV-infected men and women, immunocompromised men and women, women with a history of cervical or vulvar cancer (or high-grade cervical lesions), and women participating in receptive anal intercourse
Over the last 10 years, the rate of new anal cancer cases has been rising on average 2.2% each year. Approximately one million people are diagnosed with anal cancer globally each year. Uganda is a developing country with an estimated total population of 34 million and the incidence of anal cancer is reported to be low however this gives a clinical impression is that it occurs predominantly in young people. We must be vigilant; we are trying to create a culture where we take away the taboo, demystify and destigmatize as we hope for a community of people who are health conscious and are comfortable in their own skin enough to ask the right questions.
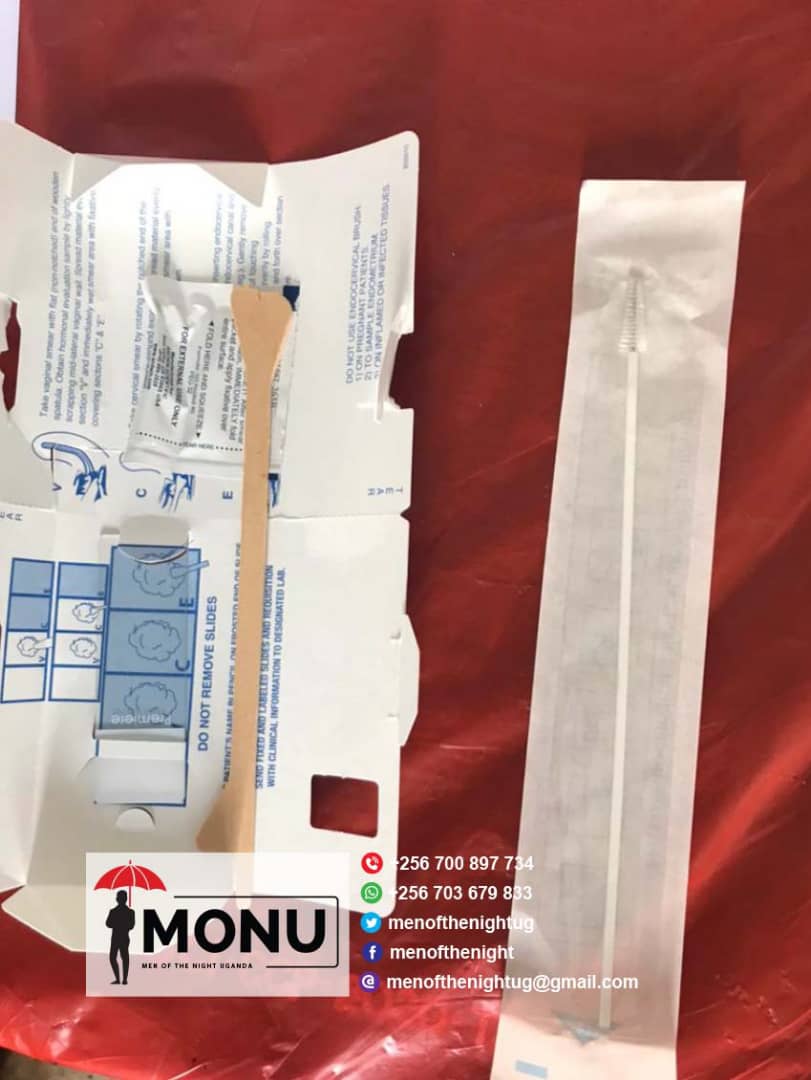
The lingering question we know you have from reading thus far is, “How is an anal pap smear done?” It’s as simple as two swabs. These swabs should be done with a Dacron swab that looks like a Q-tip, not a brush like the one used for cervical pap smears. Each swab is swirled in the anus to collect cells, which are then deposited onto slides for testing and analysis. The first swab is used to look for the presence of abnormal cells, which are then graded on their level of abnormality. The second swab tests for strains of HPV, and, in this case, specifically the high-risk strains 16 and 18, which have both been linked to anal cancer. If your test results show abnormal cells and you test positive for one of the high-risk strains, you then have a few options. The most common next step is a test called a high-resolution anoscopy (HRA), in which your doctor dyes your anal cavity to highlight the areas of abnormal cells.
We often are more afraid of the results that come after screening and console ourselves with statements like, “what I don’t know, won’t kill me!” Screening is not a death sentence as perceived and if indeed found with anal cancer there are options. Men of the Night Uganda invites all people engaging in receptive anal sex to come for this screening at the various venues they will be announcing in this campaign. You can also reach MONU directly on email at menofthenightug@gmail.com or call/WhatsApp 0703679833